The National Science Foundation has awarded $550,000 to fund a collaborative new research project to develop a noninvasive, computational modeling technology for assessing the likelihood of a heart attack in patients with high levels of plaque buildup in their arteries — the primary cause of heart attack in the U.S. today.
Despite the major role it plays in heart attacks, noninvasive identification of vulnerable plaques remains an unsolved problem in cardiovascular disease. But engineers at The University of Texas at Austin may have found a solution and, through collaboration with an industry partner, will develop better and more cost-effective noninvasive diagnostic procedures and treatment options.
When our diet consists of too much fat, fatty acids known as lipids can collect on the walls of the heart’s arteries, causing a type of plaque to form that restricts blood flow to the muscle of the heart. Two-thirds of all heart attacks are caused by this plaque buildup.
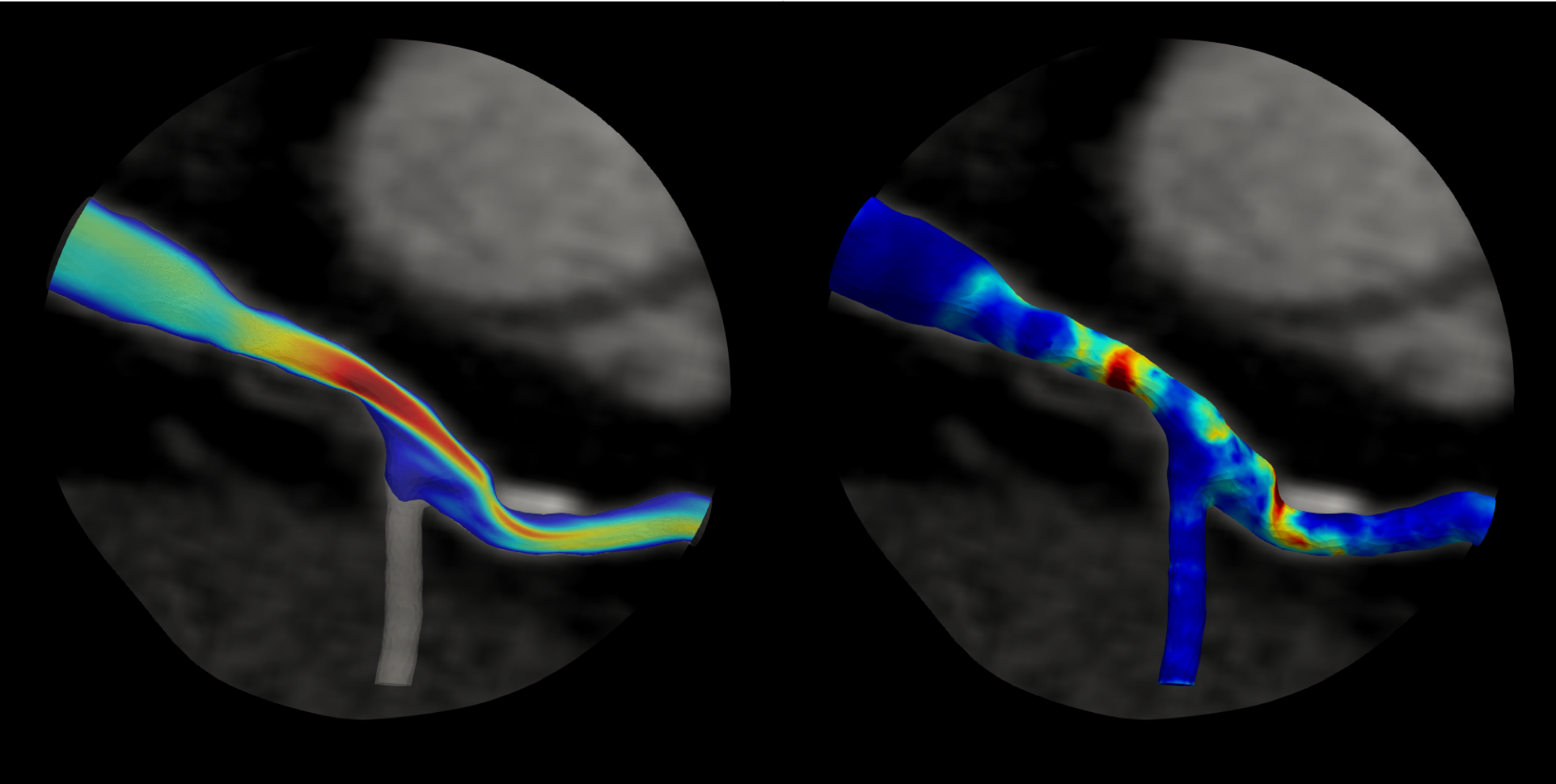
New funding will enable researchers to better understand blood flow (left) and pressure gradient (right) in heart artery blockages. Credit: HeartFlow
Cardiovascular disease is the leading cause of death worldwide. Although the treatment of coronary artery disease has progressed significantly in recent decades, the numbers of heart attacks and deaths resulting from it are increasing, due primarily to the aging population.
The new technique is being developed by project lead Thomas Hughes, professor in the Department of Aerospace Engineering and Engineering Mechanics and leader of the Computational Mechanics Group in UT’s Oden Institute for Computational Engineering and Sciences, in partnership with HeartFlow Inc., a company focused on transforming how cardiovascular disease is diagnosed and treated.
The partnership aims to create the first method to noninvasively analyze and study individual patients’ vulnerability to plaque rupture, which can suddenly trigger a clot that is large enough to block a coronary artery and cause a heart attack.
“We have an opportunity to provide a solution to an enormous unmet need, improving diagnosis, prognosis and treatment protocols for coronary artery disease, thereby preventing heart attacks and saving lives,” Hughes said.
The computer simulation technology developed through this project will be tested using prior data collected from patients who have had noninvasive assessments before a subsequent plaque rupture that led to a heart attack. In the future, risk assessment using this informed modeling technique can then be performed on an individual basis to provide physicians with guidelines for evaluating the risks of heart attack for their patients.
“Recent breakthroughs have presented the opportunity to segment vulnerable plaques from CT scans and identify material constituents, including lipid and calcium content, and fibrous caps, from which patient-specific, computational models can be formulated and the biomechanical stress in the plaque calculated,” Hughes said.
The project could also provide a blueprint for accelerating the research-to-commercialization process of novel health care technologies.
Successfully and efficiently transferring medical technology from the lab to real-world clinical settings historically has been difficult. Because of the strict guidelines around the use of any new health-related tool, the process of conducting clinical trials and obtaining clearance from the Food and Drug Administration (FDA) can often take years to complete. However, HeartFlow is committed to pursuing clinical trials, FDA clearance, bringing the product to the clinic and commercializing it as efficiently as possible.
“The collaboration with Professor Hughes’ team at The University of Texas at Austin is a natural next step from our EMERALD study, which found that understanding the change in hemodynamic forces or stress across the plaque significantly improved identification of plaques at risk of rupture,” said Charles A. Taylor, founder and chief technology officer at HeartFlow and a co-principal investigator on the grant.
The new insights gained from this project will integrate lesion geometry, plaque characteristics and hemodynamic (blood flow) forces into a biomechanical stress analysis aided by deep-learning artificial intelligence methods and could lead to improved noninvasive simulation-based tests to better identify coronary artery plaques at risk of rupture in individual patients.
The University of Texas at Austin is committed to transparency and disclosure of all potential conflicts of interest. The university investigator who led this research, Thomas Hughes, has submitted required financial disclosure forms with the university. Hughes has an equity stake in Heart Flow, Inc., the company working with the university to commercialize the research.